
the dementia seizure spectrum™
A practical, research-informed framework for recognizing the “hidden” signs.
The Dementia Seizure Spectrum™ (DSS) helps families and clinicians make sense of the brief, confusing changes that often get overlooked in dementia care.
It connects what you see in daily life—the sudden pauses, the blank looks, the unusual movements—with what research tells us about how seizures actually appear in the aging brain.
The Four Domains of the Spectrum
The DSS organizes the confusing changes you see into four clear categories.
These are not stages of severity, and they are not a progression model. They are simply different ways that neurological events appear, giving you a structured way to observe and describe them.
1. Subclinical Activity
- What it is: Electrical changes in the brain that may not have obvious physical signs.
- In Practice: You might notice brief pauses in conversation or moments where the person seems unexpectedly distant. They may stop speaking mid-sentence or appear to “drift off” for a few seconds before returning to exactly where they were.
2. Subtle Behavioral Events
- What it is: Short episodes often mistaken for inattention or dementia progression.
- In Practice: You may observe a blank look, a momentary lack of responsiveness, or a sudden shift in awareness where they seem disconnected from the room.
3. Motor Phenomena
- What it is: Small or sudden movements that seem new or unusual.
- In Practice: This includes rhythmic jerks, subtle twitching, brief stiffness, or repetitive motions (like picking at clothes, chewing, or rapid blinking) that look like restlessness but happen in a cycle.
4. Recognizable Seizures
- What it is: The more noticeable events that clearly look medical.
- In Practice: This includes sustained repetitive movements, stiffening, shaking (convulsions), or a sudden and obvious change in consciousness that requires immediate safety steps.
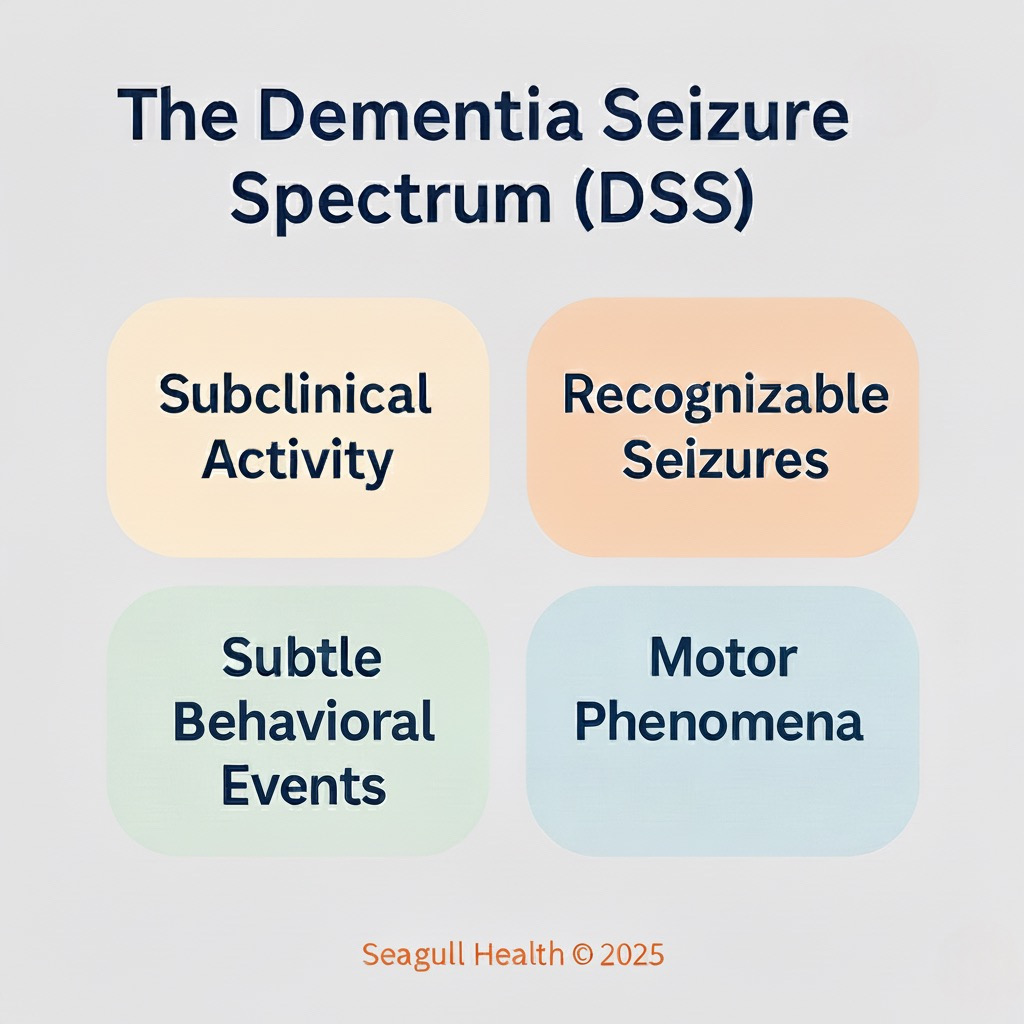
The DSS is a structured framework that describes how seizure activity may appear in dementia. It organizes observable and clinically meaningful seizure-related changes into four domains. These domains do not represent stages or severity. They support clearer observation, improved pattern recognition, and more consistent communication between caregivers and clinicians.
Why We Need a Shared Language
Without a framework, important clues are missed. The DSS helps by:
- Organizing Observations: Turning random “weird moments” into a clear model.
- Improving Recognition: Helping you spot meaningful patterns sooner.
- Supporting Communication: Giving you the right words to use when behaviors change suddenly.
- Connecting the Dots: Linking what you see at home with what doctors know clinically.
- Reducing Confusion: Replacing inconsistent descriptions with clear terms.
- Highlighting Risks: Flagging the specific events that require clinical attention.
the four domains
These categories are not for assigning labels during care. DSS offers a structured way to understand and describe the types of neurological changes that may appear in dementia.
Subclinical Activity
In Practice
ou might notice brief pauses in conversation or moments where the person seems unexpectedly distant. They may stop speaking mid-sentence or appear to “drift off” for a few seconds before returning to exactly where they were.
Clinically
Often associated with electrical irritability in the brain that produces no visible motor signs.
Subtle Behavioral Events
In Practice
Short episodes often mistaken for inattention. You may observe a blank look, a momentary lack of responsiveness, or a sudden shift in awareness where they seem disconnected from the room.
Clinically
Consistent with focal impaired awareness seizures. These often overlap with behaviors labeled as apathy, sundowning, or disorientation.
Motor Phenomena
In Practice
Small or sudden movements that seem new or unusual. This includes rhythmic jerks, subtle twitching, brief stiffness, or repetitive motions (like picking or chewing) that look like restlessness but happen in a cycle.
Clinically
May reflect myoclonus, focal motor activity, or short tonic movements.
Recognizable Seizures
In Practice
The more noticeable events that clearly look medical. This includes sustained repetitive movements, stiffening, shaking, or a sudden and obvious change in consciousness.
Clinically
Includes focal or generalized motor seizures with identifiable clinical features.
The Challenges of Recognition
Seizure activity in dementia is notoriously difficult to spot because:
- Vague Patterns: Without structured notes, the pattern remains invisible.
- Episodes are Brief: Events often last only 30–90 seconds.
- Mimicry: Signs often look like “zoning out” or general confusion.
- Quick Recovery: The person often returns to normal quickly, leaving you doubting if it happened.
- Inconsistent Views: Different family members or staff might see different things at different times.
From Theory to Practice
The DSS is the clinical backbone of our SeizureSafe programs.
SeizureSafe Academy
We translate these clinical domains into plain language, giving you the video examples and log sheets you need to track “Subtle Behavioral Events” or “Motor Phenomena” at home.
SeizureSafe Pro
We use the DSS to train nursing staff on clearer observation and consistent communication, reducing the risk of missed diagnoses in senior living.
Important Clinical Note
- Not a Diagnosis: The DSS helps you describe what you see; only a doctor can diagnose a seizure disorder.
- Not a Staging Model: Being in one domain does not mean the condition is “worse” than another.
- Not a Replacement: This framework does not replace a full medical evaluation.
- Not a Predictor: Using this framework does not predict future severity or outcomes.
Learn to Recognize The Patterns
The best way to understand the DSS is to see it in action.
